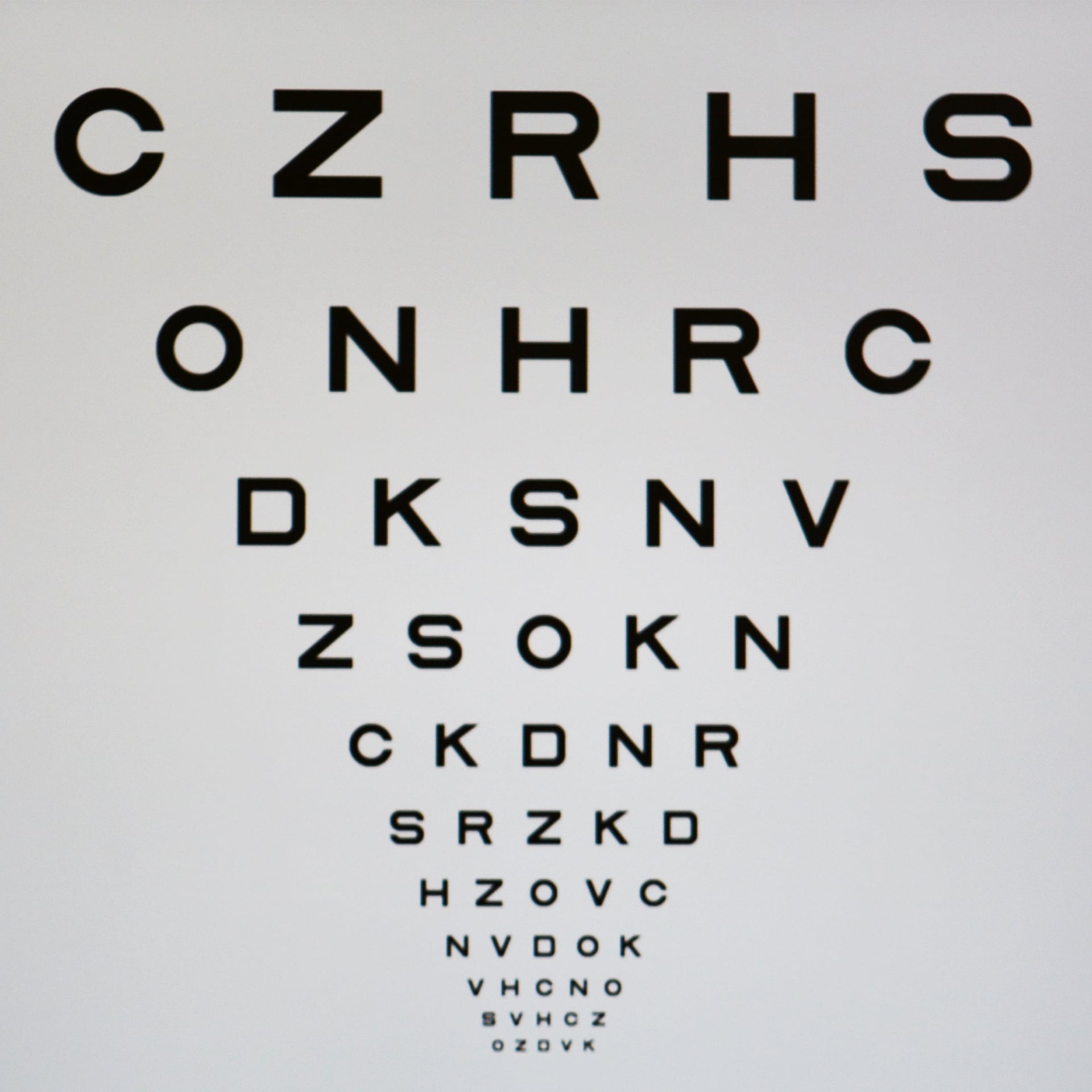
Get Help Preserving Your Eye Health
Your eye health is far more important to manage than you may realize. About 93 million Americans have a high risk of experiencing vision loss due to eye disease, many of which can develop with no noticeable early symptoms.
We’re committed to using leading technologies and techniques to detect these issues before they damage your vision. You can start serving your eye health by having an eye exam today. The earlier we can detect and diagnose an eye problem, the better we can manage its effects.

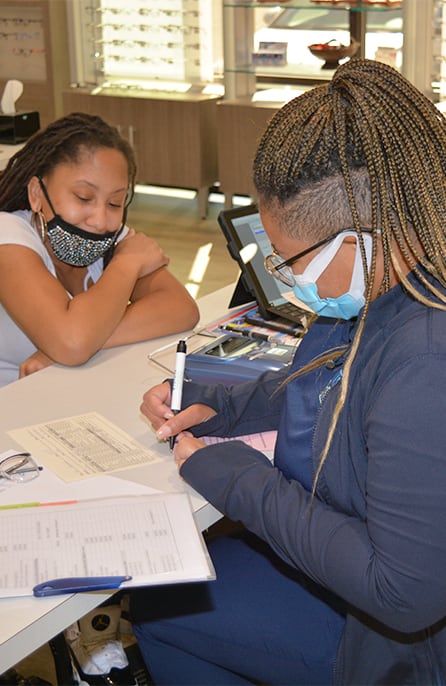
How We Detect Eye Health Problems
Vision Therapy Institute is proud to use state-of-the-art technology to search for signs of eye diseases before they have a chance to affect your vision. We use these tools during every comprehensive eye exam, ensuring that everybody we help gets the same detailed look into their eye health.
Some of these tools include:
- Optos ultra-widefield retinal imaging
- Goldmann applanation tonometry
- Non-contact tonometry
- Icare tonometry
- Virtual Field
During your exam, we’ll have a conversation with you about your health history and your family’s health history. This information helps our doctors determine if you have a higher risk of developing eye issues.

Common Eye Diseases & Conditions
The risk of developing an eye disease ranges from person to person. Genetics, health conditions, and your overall lifestyle can all factor into your eye health. However, one of the most common risk factors is age—aging increases the risk of several eye diseases and conditions that could permanently affect your vision.
We recommend eye exams every 2 years for adults 18 to 64 and annually for seniors 65 and up. If you have a high risk of developing an eye disease, we may recommend more frequent eye exams.
Glaucoma
Glaucoma is a group of eye diseases that damage the optic nerve over time. Generally, glaucoma occurs when your intraocular pressure (IOP) increases, but other forms of glaucoma can also develop without raising your IOP.
Glaucoma has no cure and can cause vision loss as it damages your optic nerve. However, our team can detect glaucoma by measuring your IOP levels or observing your optic nerve during a comprehensive eye exam.
Age-Related Macular Degeneration
Age-related macular degeneration (AMD) is an eye disease that slowly thins your macula over time, leading to vision loss. Your macula is the centermost part of your retina, responsible for providing the sharp detail you need to read, drive and recognize faces.
AMD commonly affects people over the age of 50, and the risk of developing it can increase if you smoke or have a family history of the disease.
Diabetic Eye Diseases
Diabetes can increase the risk of several eye diseases and conditions, including glaucoma, cataracts, and diabetic retinopathy. If you have diabetes, we recommend annual eye exams to detect issues before they affect your vision.
Check out our Diabetic Eye Exams page for more information!
Cataracts
Cataracts are the leading cause of blindness globally. Cataracts are a condition that clouds your eye’s lens over time, occurring when proteins on your lens clump together and make your lens more rigid. The result is a hazy, milky look that affects your vision quality.
Cataracts generally develop through the aging process, and the risk of developing them increases if you smoke, drink excessively, or have diabetes. Glasses and contacts can correct early vision errors caused by cataracts, but only surgery can effectively treat cataracts.
Find Out How We Can Help
The road towards managing and preserving your eye health begins when you come in for an eye exam. Our team is ready to help you today, and all you have to do is request an appointment.

Our Location

OUR ADDRESS
- 3618 Sunset Blvd, Suite A
- West Columbia, SC 29169
CONTACT INFORMATION
- Phone: 803-732-4099
- Fax: 803-227-8992
- Email: [email protected]
Office Hours
- Monday: 9:00 AM – 6:00 PM
- Tuesday: 10:00 AM – 6:00 PM
- Wednesday: 9:00 AM – 6:00 PM
- Thursday: 9:00 AM – 6:00 PM
- Friday: 9:00 AM – 1:00 PM
- Saturday: Closed
- Sunday : Closed
Our Brands